Today, around 40 million Americans dedicate themselves to providing unpaid care to an adult or child (this includes Veterans), navigating the complex responsibilities that come with caregiving. But what will caregiving look like in the near future? As someone who has been in the industry since my mom first started working in a nursing home when I was 3 years old and having worked at all levels of senior care and owning a home care agency today, I have been wondering what the future of caregiving will look like in the future.
Advancements in technology, evolving policy frameworks, and significant demographic shifts are poised to redefine what it means to care both for families and professional caregivers. Let’s look at the future trends in caregiving and their implications for caregivers and care recipients alike.
Looking at today’s caregivers, they provide critical support that ranges from personal care to medical tasks, with the vast majority of care recipients being adults aged 50 or older. According to the AARP’s “Caregiving in the U.S. 2020” report, the average caregiver is a 49-year-old woman who works outside the home and spends nearly 24 hours per week providing care to her mother.
Economic Impact of Caregiving
The economic value of the unpaid care provided by these individuals is staggering. The AARP also notes that in 2023, the estimated economic value of caregivers’ unpaid contributions was nearly $600 billion, which exceeds the annual sales of the four largest U.S. tech companies combined. This underscores the critical economic role that family caregivers play, often at significant personal and financial cost.
Health Impact on Caregivers
The personal impact on caregivers is profound, particularly in terms of health and wellbeing. A study by the National Alliance for Caregiving and AARP found that 21% of caregivers report higher levels of physical strain, and 21% consider caregiving a cause of emotional stress. Caregivers are at a higher risk for a range of health issues, including depression, anxiety, and cardiovascular disease, due to the chronic stress associated with caregiving tasks. Caregiver burnout is real.
Impact of Caregiving on Families
Financial Strain
Caregiving can place a significant financial burden on families. According to the same AARP report, out-of-pocket costs for caregivers average about $7,242 annually, which includes expenses related to medical care and daily living needs of the care recipient. For families living at or below the median household income, these costs represent a substantial portion of annual earnings, often leading to financial instability. This is where I wish more communities offered and more people knew about medical lending libraries.
Work and Career Impact
The demand of caregiving responsibilities also significantly affects employment. Approximately 61% of caregivers experience at least one change in their employment due to caregiving, such as reducing hours, taking unpaid leave, or receiving a warning about performance or attendance. Women, in particular, are more likely to report adverse effects on work life, which contributes to a gender gap in income and career advancement directly linked to caregiving duties.
Family Dynamics and Relationships
While caregiving can strengthen bonds between family members, it can also strain or break relationships. Caregivers often feel isolated and unsupported, particularly if they are “solo” caregivers without assistance from other family members.
Emotional and Social Consequences of Caregiving
The emotional toll of caregiving is considerable, with many caregivers reporting feelings of isolation, anxiety, and depression. Social activities and personal hobbies often take a backseat, affecting the caregiver’s overall quality of life and mental health. Moreover, caregivers providing high-intensity care are particularly vulnerable to emotional distress and social isolation.
Understanding these impacts can help shape better policies and support systems for caregivers, ensuring they receive the necessary resources and recognition for their vital contributions. As we consider the future of caregiving, it’s essential to address these challenges to not only support caregivers but also to sustain the caregiving infrastructure that so many families rely on.
Technological Advancements for Caregivers
Smart Home Technologies
The integration of technology into home care is rapidly transforming caregiving. By 2025, nearly half of all elderly persons are expected to use at least one smart home device. These devices, ranging from automated lighting systems to advanced sensors that monitor health and activity levels, play a crucial role in enhancing safety and comfort, promoting independence, and reducing the need for constant physical supervision.
Wearable Health Monitors
Wearable technologies are not just fitness trackers; they are life-savers. These devices continuously monitor health vitals such as heart rate, blood pressure, and blood sugar levels, significantly reducing hospital visits by 25% by enabling early detection and management of potential health issues. As technology evolves, these wearables will become even more sophisticated, providing real-time data to caregivers and healthcare providers. Even devices like Cardio.io, which can detect irregularities in heart rate, breathing rate, stress levels & sleep quality allows caregivers to receive text alerts within 60 seconds if the heart rate dips or spikes are changing how we monitor and care for family. All this with no wearables and no contact, by using radar sensors and a smartphone app.
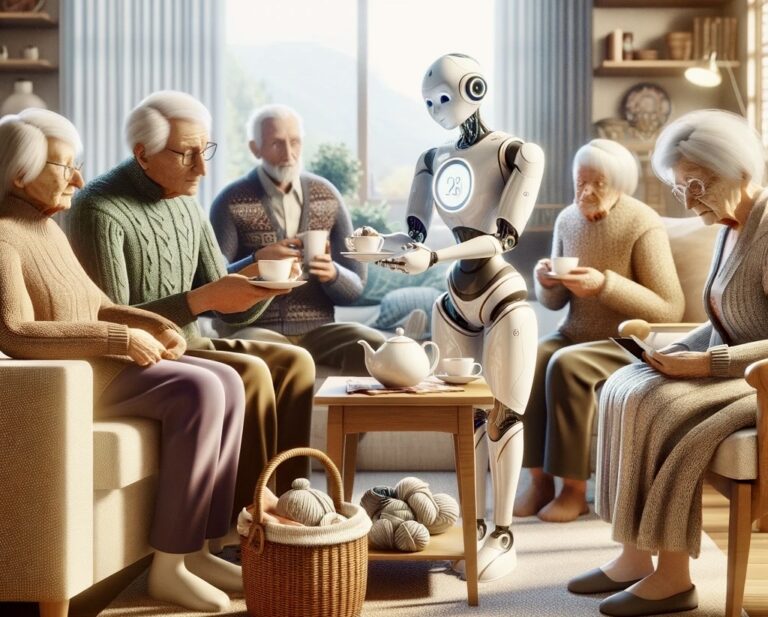
Robotics and AI in Caregiving
The elder care robotics market, projected to reach $3.25 billion by 2025, includes innovations from companionship robots to automated mobility aids. These robotic solutions offer not just physical assistance but also companionship, helping to alleviate the emotional toll of aging and loneliness.
Japan, with its rapidly aging population and shrinking workforce, has been a pioneer in adopting robot caregivers. Given that more than a quarter of its population is over 65, Japan has turned to technology to fill the gap in elderly care.
Robots like *Robear*, developed by RIKEN and Sumitomo Riko, have capabilities that include lifting patients from beds into wheelchairs, helping to reduce the physical strain on human caregivers. Another example is *Paro*, a therapeutic robot designed to look like a baby seal, which is used to provide comfort and emotional support to elderly patients. Paro has been shown to reduce stress and improve relaxation among its users.
In the United States, the use of robotic caregivers is still in the early stages compared to Japan, but interest is growing. Robots such as *Moxi*, developed by Diligent Robotics, are designed to assist in clinical settings by autonomously performing tasks like gathering supplies or delivering lab samples. This allows human staff to focus more on patient care rather than logistical tasks. While direct caregiving robots are less common, the U.S. market is seeing increasing integration of robotic technology to support the caregiving sector.
AI is set to transform caregiving by enhancing both the capabilities of robots and the tools available to human caregivers. Here’s how AI is contributing to caregiving:
Predictive Care: AI algorithms can analyze data from various sources, including wearable devices, to predict health events before they occur. For example, AI can detect changes in a person’s gait or sleep patterns that might indicate a risk of falling, allowing for preventative measures to be implemented proactively.
Personalized Care: AI can help personalize the care routines for individuals based on their specific needs and preferences, learned over time through interaction patterns. This personalization can increase the effectiveness of care and improve the quality of life for recipients.
Communication Aids: AI-powered tools like voice assistants and chatbots can help overcome communication barriers. They can provide social interaction for the elderly, help them stay connected with family and friends, or remind them of medications and appointments.
Automation of Routine Tasks: AI can automate routine tasks such as scheduling, monitoring medication adherence, and maintaining records of health metrics. This automation frees up human caregivers to spend more quality time with care recipients and focus on more complex care needs.
Emotional Recognition: Advanced AI systems are being developed to recognize emotional states from facial expressions, voice intonation, and body language. These systems can alert caregivers when a patient may be feeling sad, anxious, or in pain, often before they communicate it verbally.
Future Implications of Caregiving Automation
The integration of robotics and AI into caregiving presents a promising avenue to address the growing care demands of an aging global population. However, it also raises ethical and practical considerations about dependency, privacy, and the changing nature of the caregiver-patient relationship. As these technologies advance, they must be developed and implemented thoughtfully to enhance human caregiving rather than replace the essential human touch. If these robots can help in the common tasks where caregivers are at risk for injury for example, that would be a terrific advancement.
As we continue to explore these technologies, the goal remains to support caregivers and improve the independence and well-being of those in need of care, creating a balanced approach between technology and human compassion.
Policy and Regulation Changes
Government Policies
With the aging population growing, there is a pressing need for policies that support caregiving. Initiatives are underway to expand Medicare to cover more home health services, recognizing the shift towards in-home care over institutional care. These policies aim to improve the standard of caregiving and make services more accessible.
Some of the major federal initiatives aimed at supporting family caregivers in the United States include:
1. The National Strategy to Support Family Caregivers
– Originating from the RAISE Family Caregivers Act of 2018, this strategy outlines a comprehensive approach to enhance public awareness, support systems, and services for family caregivers, involving both governmental and private sector actions.
2. Public Health Emergency (PHE) Acute Hospital Care at Home (AHCaH) Waiver
– This CMS waiver expands the Hospital at Home model to provide acute hospital-level care at home, reducing hospital strain and improving patient-centered care.
3. Supplemental Benefits under Medicare Advantage
– Since 2019, Medicare Advantage plans have more flexibility to offer expanded supplemental services, including support for caregivers and long-term support services (LTSS), tailored to individual care needs.
4. American Rescue Plan Act of 2021
– This act boosts funding for Medicaid home- and community-based services (HCBS), addressing HCBS workforce issues, expanding service capacity, and reducing waitlists to better support caregivers and their recipients.
5. Spousal Impoverishment Protections
– These protections prevent the financial impoverishment of the spouse of a Medicaid recipient, allowing them to retain a part of their assets and income.
6. Expanded Supports for Caregivers of Veterans
– The VA MISSION Act of 2018 broadened the VA Program of Comprehensive Assistance for Family Caregivers to include pre-9/11 veterans, offering various supports to caregivers, including financial and health services.
Insurance and Coverage
Recent years have seen a shift in insurance policies to include broader coverage for non-medical home care services. This change is vital as it acknowledges the importance of comprehensive long-term care, which includes everyday assistance, not just medical care.
Social Shifts
Increasing Demand for Professional Caregivers
As of 2030, 20% of U.S. residents will be of retirement age, a statistic that underscores the growing demand for professional caregivers. This demographic trend suggests a booming market for caregiving services, pushing communities and businesses to innovate and expand capacity to meet this demand. I’ve witnessed the explosion of new senior (55+) communities and care residences in the last few years as our population ages.
Changing Family Dynamics
The traditional family caregiving model is under pressure as family sizes decrease and the geographical spread of family members increases. More people are turning to professional caregivers to fulfill roles that family members once managed, indicating a shift towards formal care arrangements.
Workforce Development
Training and Education
To equip caregivers with the necessary skills, educational institutions are increasingly offering specialized programs. These range from certifications in geriatric care to advanced degrees in elder care management, reflecting the complexity and importance of caregiving roles.
Employment Opportunities
The caregiving sector is expected to see a 36% increase in job openings for home health aides by 2028, highlighting not only the need for more workers but also the vast opportunities for those seeking a career in this field. We’re always hiring amazing caregivers.
Caregiving’s Future
The future of caregiving is poised at the exciting intersection of technology, policy, and demographic trends. Each element offers a piece of the puzzle in enhancing the caregiving experience, making it safer, more efficient, and more compassionate. As we look forward, it’s clear that embracing these changes will not only improve the quality of care but also the quality of life for our aging population. I have been around the senior care industry nearly half a century, and I hope as we think about the impact of technology on caregiving for seniors, the one thing that should be constant is the need for the human capacity of caring and incredibly compassionate caregivers. While technology can mimic empathy and caring, it is no substitute for the human touch.

From a young age, Stacey’s link to the senior care industry grew alongside her mother’s work at a nursing home, where she often accompanied her. By her early teens, she secured her first official job at a nursing home, laying the foundation for a profound journey in senior care spanning over four decades. Her roles varied from opening assisted living and memory care residences to working in nursing homes and independent senior living communities. As the former Director of Fun for 300 independent seniors, she expertly organized daily events and trips. Stacey’s unwavering passion, nurtured by her family, and professional dedication as a recreation therapist, reflect her deep commitment to preserving the dignity and well-being of seniors.
Stacey’s senior care expertise has been recognized by the media including U.S. News and World Report and Care.com.
Stacey and her husband Bryan are the owners of the senior in-home care agency A Place At Home – North Austin.